Living with Dementia: Your Essential Guide

In this guide, we’ve shared expert views, practical advice and personal stories on navigating life with dementia. Whether you’ve been diagnosed yourself, or have taken on the caregiver role of someone who has, discover how to live well after diagnosis and maintain your quality of life, for as long as possible.
What is dementia?
Dementia is caused when the brain is damaged by diseases. It is progressive, meaning the symptoms will eventually get worse, and current treatments are limited and only suitable for certain types of dementia. The word is an umbrella term covering many different types of the condition – and while experts don’t have an exact figure of how many there are, it’s estimated to be over 100, which each type having a range of different symptoms. Dementia can affect anyone, whatever their gender, ethnic group, class, educational or professional background,
This all means your individual symptoms of dementia may differ greatly to someone else’s.
Coping with a dementia diagnosis
Living with dementia has a big emotional, social, psychological and practical impact. Indeed, it is often said that it’s not just the person who is diagnosed, but everyone who knows and loves them that goes through a wave of emotions and challenges.
There’s no right and wrong way to react to a dementia diagnosis. You and your family may feel relieved to have an explanation for worrying symptoms, or you may feel like you’re going through something akin to a grieving process.
You’ll likely need to go through a period of adjustment after the diagnosis, and may struggle to accept it, even if the clinical reasons have been clearly explained.
There are many different emotional reactions, and it’s important for everyone affected to acknowledge those emotions, and seek help and support if you feel you need it. If you’re looking for outside support, the following helplines can be a good place to start.
Tommy’s diagnosis story
Campaigner Tommy Dunne was diagnosed with Alzheimer’s at the age of 58. He’s kindly shared his experience of being diagnosed with us, as well as an important message to those looking to learn more about life with dementia.
 Prior to diagnosis, I had gone to work one day, and I was having a meeting with one of the directors and some senior managers when (so my wife was told) I just glazed over, stood up without saying anything and left the building – and must have walked home.
Prior to diagnosis, I had gone to work one day, and I was having a meeting with one of the directors and some senior managers when (so my wife was told) I just glazed over, stood up without saying anything and left the building – and must have walked home.
When my wife came home, she saw my jacket by the front door and my clothes on the stairs and found me sobbing under the bedclothes. She took me to the doctor who said it looked like I’d had a breakdown, so I was put on antidepressants and given a note to stay off work.
Over the following weeks, I became worse and was referred to a psychologist and then a psychiatrist, who diagnosed me as bipolar and prescribed lithium. My wife was adamant that I wasn’t bipolar though, and I was eventually referred to see a different psychiatrist who gave me another five months of tests and brain scans.
He then visited me at home and told me, “I’ve some good news for you and some bad news: the good news is you don’t have bipolar, the bad news is you have Alzheimer’s”. My first thought was, “That can’t be. I can think, I can function”.
As soon as I heard the diagnosis of dementia, I became afraid. Fears went through my mind, about being still able to think but not being able to communicate with my family. I withdrew into myself. Daily life became staying in bed till late, watching daytime TV and going to bed early. That was what I thought someone did when they had Alzheimer’s – and that you could not contribute anything to society.
My wife and I had been keen golf players, and I told her that she needed to play and get out of the house because I’d started to notice the energy draining out of her. One morning I was watching TV, feeling particularly low, when she came in and took one look at me and said, “I’m not having this, you’re going back to the golf.”
I thought that everyone would be looking at me, and refused to go into the club house initially but I surprised myself as I could still play to a good standard at that time.
When I went to the club house for the first time after being diagnosed, I realised that when you get dementia, you gain a super power; the ability to become invisible. My wife’s friends would have a full conversation about me as if I wasn’t there. “It must be awfully hard for you”, they would say to her.
If you want to learn what it really is like to live with dementia, then you have to ask a person with dementia to tell you – and be open to the answers.
Dementia in younger people
People with dementia whose symptoms started before they were 65 are described as having ‘younger-onset dementia’. There are estimated to be at least 42,000 people living with this kind of dementia in the UK.
The symptoms of dementia may be similar regardless of a person’s age, but younger people often have different needs – they may, for example still be working when they’re diagnosed – and therefore require age-appropriate support.
Dementia in a younger person can progress more rapidly, although this may be partly down to our perceptions – if your loved one has found it more difficult to get a timely diagnosis due to their age, their dementia may have significantly progressed by the time they are eventually diagnosed with dementia.

Treatments for dementia
There’s no cure for dementia. Treatment is all about managing symptoms and making life as fulfilling as possible. This goes beyond simply drug treatments. Talking and alternative therapies – such as music and reminisce are increasingly popular ways of coping with the condition.
Many people living with dementia, and indeed people not living with dementia, register for join dementia research to contribute towards understanding of dementia, support the discovery of new treatments and help in working towards a cure.
Complementary therapies
Complementary therapy might help a person manage some of the common symptoms of dementia – these might include feelings of agitation, tiredness, or being unable to concentrate.
Some examples include –
- life story work – this is where a person with dementia is encouraged to reflect on their background, interests, and who and what is important to them, creating a ‘fact file’ that can be shared with family and friends to help them understand them better. it’s sometimes offered as a course through a memory clinic after diagnosis.
- music – this can involve listening to certain pieces of music to spark memories, dancing, or singing in a group or choir such as Singing for the Brain).
- sensory stimulation – this focuses on communicating and evoking feelings through the senses rather than relying on a person’s thinking ability. It may include things like acupuncture, aromatherapy and massage.
If you or your loved one isn’t offered any non-drug treatments after diagnosis either from the memory clinic or the GP, you may need to research qualified therapists in your local area, or look out for adverts for dedicated classes or groups on online directories, or in community spaces.
The importance of preserving memories
When a person develops dementia, they may begin to lose their memories of important aspects of their life. This doesn’t mean a person cares any less about them.
More recent memories often go first, while distant ones remain for longer. The items we collect in our lifetimes are an important link to them all, and can be used to create life story resources. Think photo albums, collage photo frames, a memory book (which could include a family tree or timeline), a memory box with lots of small mementos, or a memory board.
You can personalise anything with images from your own or your loved one’s life, even blankets. And if you or your loved one is comfortable with technology, there are lots of life story apps such as The Inspired App, available for iPads and similar devices. With this sort of technology, you also have the option to make audio recordings or videos.
Life story resources are particularly useful when a person needs professional care, as they can help care workers better understand a person – their history, special moments, likes and dislikes.
To find out more about creating life stories, there are a number of useful resources and templates available, including –
Making changes to the home
One of the most important ways a person with dementia can feel safe and supported is through their home environment. Consider, does your or your loved one’s help them live their life well? Does it compensate for any difficulties, like disorientation and confusion? Does it maximise independence in a safe way?
Before you make any changes to a loved one’s home, talk to them about what is working for them and what isn’t. Be mindful not to make wholesale changes in one go, as this might add to any confusion your loved one is experiencing.
Some of the key ideas you might want to discuss are:
- Really make it home: A meaningful and recognisable interior design, incorporating your loved one’s life story, with signage (signs that combine pictures and words). An open-plan layout to help with navigation, and use of different colours to help with understanding.
- Add the right signage: Instructional signs can help with completing simple tasks. Labelling essential kitchen cupboards can be helpful too, as can installing bathroom signs, such as those you find in public places to help with finding the toilet.
- Remove confusing surfaces: Covering reflective areas, laying plain and consistent flooring (avoid mats and rugs, which can look like a hole in the floor) and removing bold patterns (such as a flowery tablecloth that could look like actual flowers)
- Get the light and sound right: Good natural lighting to reduce glare and shadows. Be mindful of light pollution into your the bedroom at night, and of minimising echoes and noise pollution. Consider setting maximum volumes for TVs and radios to minimise sudden loud noises.
- An accessible garden: think handrails, well-lit seating areas, raised beds and sensory stimulation from plants.
For more suggestions for creating a safe and comfortable environment can be found in our guide to creating a dementia friendly home.
There may also be local carers groups in your area that offer advice. These are often run by national charities like the Alzheimer’s Society, or local charities. TIDE (Together In Dementia Everyday) offers a peer support network for carers of those with dementia.
More practical things to consider
There’s rarely any need to make big change overnight after a dementia diagnosis. However, it’s worth starting to think about some lifestyle aspects that are going to change, or daily activities that are likely to become harder over time – and making sure as family, you’re ready.
Driving and dementia
When diagnosed with dementia, a person will need to make sure they inform both the Driver and Vehicle Licensing Agency (DVLA) and their insurance company.
If you drive and you don’t want to surrender your licence, your doctor will need to compile a medical report on how fit you are to drive. Your licence may be revoked, you may need to be retested, or your licence will be renewed for a fixed duration before another review.

Diet
Be aware that changes in eating habits. Taste buds may change too, and you may notice a preference for sweet or finger foods. Be mindful, too, of swallowing difficulties – known as dysphagia as dementia progresses too.
Hydration is also important. Dehydration may cause someone to become more confused, and increase the risk of a urinary tract infection (UTI). The Eatwell Guide offers advice on recommended levels of hydration and how to achieve them.
Did you know?
 There are over 300,000 people over 65 who are vegan or vegetarian. In fact the UK Vegan Society was itself founded in 1944. If you’re plant based, you may worry what will happen when you can no longer cater for yourself. Amanda Woodvine, Chief Executive of charity Vegetarian for Life, offers the following advice –
There are over 300,000 people over 65 who are vegan or vegetarian. In fact the UK Vegan Society was itself founded in 1944. If you’re plant based, you may worry what will happen when you can no longer cater for yourself. Amanda Woodvine, Chief Executive of charity Vegetarian for Life, offers the following advice –
- Have conversations about your dietary wishes with as many people as possible and make sure that you’ve made an advance care statement.
- Some people have recorded a video of themselves talking about their wishes for the benefit of anybody caring for them in the future. Doing something like this can also help your own memory of why you were vegetarian or vegan in the first place.
- If food is being prepared by someone who is not a vegetarian or vegan, they can find single portion recipes here, or simple 5 ingredient recipes here.
Staying socially active
People with dementia can easily become isolated. So maintaining an active social life is hugely important. Social activity works best when it involves something you enjoy and the company of like-minded individuals. You may be able to find local groups or classes to attend to support an existing hobby, or decide to try something new.
Peer support networks are particularly helpful for those living with dementia, bringing them together to share their experiences and support one another. Dementia cafes are safe spaces to meet other people in your situation, and do social activities designed to stimulate the mind and make navigating life with dementia little easier. You can find your nearest cafe here.
You can find out more by contacting the UK-based Dementia Engagement and Empowerment Project (DEEP), or the worldwide Dementia Alliance International (DAI).
Dementia and holidays
Many UK transport providers are committed to being ‘Dementia Friendly’, providing staff with Dementia Friends sessions and adapting services to cater for people with disabilities.
When using public transport services like buses and trains, you can enquire about assistance in advance if you feel this would be helpful. You can also apply to join the Blue Badge scheme for car parking.
If you’re thinking about going on a break with your loved one, there are a number of holiday providers who specifically cater for people with dementia. You can find out more about these on the Young Dementia UK website, or in our guide to planning holidays in later life.
If you’d rather make your own arrangements, make sure you consider your transport options carefully and allow yourselves plenty of time to make transfers.
Book the type of accommodation that will suit your loved one best – this may be on the ground floor, or in a room away from the road – and consider how you’ll access the food and drink that they’ll enjoy (you may need to take some from home). If you want to visit any attractions, enquire in advance if they offer specific support for people with dementia.
Remember you’ll need to make sure you have comprehensive travel insurance, and it may be helpful to ensure emergency contact details are always on your loved one’s person in case you become separated.
Getting enough sleep
People with dementia may find it affects their sleep, and feel exhausted, and perhaps irritable during the day.
This can have a negative impact on day-to-day life. For example, it may lead to sleeping more in the day, and therefore not feeling sleepy at night. Some people become disorientated, thinking it’s morning and they should be getting washed and dressed when it’s actually nighttime. Sleeping problems may be particularly acute when the clocks change. You can find out more in our guide to sundowning.
Creating healthier sleep habits
 Last year, sleep physiologist, Stephanie Romiszewski shared her expert advice on building a healthier sleep routine. Stephanie regularly shares her advice and practical tips on television and radio. She was the resident sleep expert in Channel 4’s ‘Secrets of Sleep‘ series and the BBC’s ‘Insomnia and me‘.
Last year, sleep physiologist, Stephanie Romiszewski shared her expert advice on building a healthier sleep routine. Stephanie regularly shares her advice and practical tips on television and radio. She was the resident sleep expert in Channel 4’s ‘Secrets of Sleep‘ series and the BBC’s ‘Insomnia and me‘.
- Maintain the same wake time each day, no matter how much you love a lie in.
- Get plenty of light exposure in the first two thirds of the day. Light exposure is your absolute best friend and it’s free and available to all of us.
- Eat and move as consistently as possible each day too. You can’t metabolise and sleep at the same time, so if you’re consuming calories close to when you want to sleep, you’re going to notice that your brain’s not recognising your sleep signals.
As dementia advances
While no one wants to think about crisis situations, it can help to make sure you’re fully prepared for future health problems as you or your loved one moves through the different stages of dementia.
A person with dementia may experience progressively deteriorating communication skills, dysphagia (swallowing problems) and issues with mobility and continence . These are areas of physical deterioration that family carers often find tricky to deal with alone. In fact, in our own 2023 research, providing personal care (washing, toileting) was the second biggest concern among informal caregivers aged 45 and over.
A person may also lose more weight than is usual for them, have more falls and become more vulnerable to infection. Hospital stay may become more likely, or more frequent too.
However, the rate your or your loved one’s dementia progresses is impossible to predict. Therefore it’s important to get as much preperation done as early as you can, to avoid additional stress if something unexpected happens. You may wish to complete a ‘This is Me’ document. This helps hospital staff get to know your loved one and their likes and dislikes, leading to a more positive in-patient experience. It’s also worthwhile to know about John’s Campaign, which centres on supporting families to be with their loved ones during periods in hospital.
Helping younger children understand dementia
 Dementia is difficult enough when you understand what’s happening, but for younger family members, seeing someone acting differently can be really confusing, or upsetting.
Dementia is difficult enough when you understand what’s happening, but for younger family members, seeing someone acting differently can be really confusing, or upsetting.
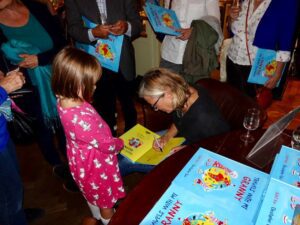
Journalist and author Juliet Rix spoke to dementia experts, carers and families and people living with dementia themselves, and wrote a book that offered children a way “into” the condition, and some sort of understanding that isn’t disrespectful of the person with dementia.
‘Travels with my Granny’ is a story about granny and her grandchild and how they go travelling around the world together. It’s aim is to help children understand that dementia symptoms don’t need to be frightening, as it simply means someone has ‘travelled somewhere else’ in their mind.
You can find out more about the book here, or read our chat with her here.
Supporting your loved one as a family
For many people living with dementia, the support of family, friends and neighbours is key to living well. If you’re providing such support, identifying yourself as a carer and seeking appropriate help is key to you being able to maintain your own health and wellbeing.
The experiences of family caregivers
As you probably well know by now, dementia doesn’t just impact the life of the person who’s been diagnosed – the emotional impact of dementia and the new responsibilities it creates can spread far wide throughout family and friends.
Being a family carer can be extremely stressful, putting a strain on you both physically and mentally.
Mental Health UK found that 73% of people agree that increased caregiving responsibilities, such as looking after elderly parents, could contribute to people buckling under the pressure and burning out.
Caregiver stress can affect people at different stages of the care journey, for example –
- When you take on the caregiver role unexpectedly, and when there is uncertainty around how long you’ll need to provide care for
- When you’re a person’s primary caregiver and lack the support or resources you need
- When the care you give doesn’t seem to be having an impact on the health or wellbeing of the person you’re looking after
- When the person receiving care is resistant to your help
In order to support to the best of your abilities, it’s important to ensure you access the services that you’re entitled to.
Under the Care Act, all family carers are legally entitled to an assessment of their needs by their local authority, which may lead to additional support. You can find out more information on your rights here, and on the assessment process here. Bear in mind you may need to be proactive and request this assessment if it isn’t automatically offered by your local authority. As a family carer, you may also be entitled to financial support from the government.
It’s also important that your GP knows you’re a carer. GPs keep a ‘carers register’, which may help you access services like the flu jab and a carer’s health check – an appointment that is just about you and your health needs. You can find out more information about how to look after yourself on the Carers Trust website.

Advance care planning
As dementia progresses, cognitive decline may mean you or your loved one becomes unable to make decisions for yourselves. Formally, this is called ‘lacking capacity’. Whilst dementia can be an alarming prospect for you to face, there are steps that can be taken – before this ability is lost to ensure wishes are recorded and acted on in the future.
To help you to begin to think about the different options available, the NHS have put together a dedicated guide. Keep in mind, of course, it’s always advisable to consult a solicitor to discuss your legal requirements.
Advance decisions and advance statements
With an Advance Decision, you can stipulate specific treatments you do not want. Medical professionals are legally bound to adhere to Advance Decisions in England and Wales. However in Scotland they’re not, but are usually still followed.
With an Advance Statement, you can make more general requests about their care. Medical professionals try to follow Advance Statements, but they aren’t legally expected to.
Although you can specify your wishes verbally, it’s preferable to write everything down following a recognised format. Bear in mind that any type of advance care planning must be done when a person with dementia still has capacity to make their own decisions, is in full possession of the facts relating to their decision and is not being influenced by anyone else.
Lasting power of attorney
A lasting power of attorney (LPA) is a legal mechanism that gives a trusted appointee the power to make decisions on your, or a loved one’s behalf if they no longer have the capacity to make those decisions. It is only applicable in England and Wales.
There are two different types of LPA: a Property and Affairs LPA (which includes financial matters) and a Health and Welfare LPA. Your loved one can make either or both, but each one must be registered with the Office for the Public Guardian, who charge for this service.
An LPA must be made when your loved one has capacity. If your loved one chooses to make a Health and Welfare LPA and gives their attorney power over life-sustaining treatments, this would override any Advance Decision. If the attorney is not given this power, any Advance Decision your loved one has made would still stand.

Dementia care services
Often those who live with dementia do so for many years, and their care and support is far more about their social needs than their medical needs. This is why people with dementia usually access social care, voluntary sector and community-based services more often than NHS services.
There are a number of different types of dementia care, including shared lives schemes, cooperatives, supported living and retirement communities. But we’ve taken a look at the most common types below.
Care homes
Care homes vary in the levels of care they provide. Residential care supports people in only a few aspects of their life, while full nursing care is similar to what you’d expect from a non-emergency hospital ward.
Moving to a care home is often permanent, but it might also be a temporary measure. This is known as respite care, and usually takes place when someone is recovering from an operation or illness, or their family needs to take a break
Staff provide meals, housekeeping services and assistance with everyday needs – dressing, mobility, personal hygiene and so on. But since the number of staff varies from residence to residence, so does the amount of one-on-one care a person receives.
Domiciliary care
This is when a professional carer intermittently visits a person in their own home – usually daily.
These caregivers can help with personal care, including washing, dressing and preparing meals. The level of support depends on the package agreed.
Home care may also happen in the form of live-in dementia care. A professional carer moves into a person’s home to help the family support them, or to provide a complete care package of care.
It’s a popular alternative to a care home, enabling a person to continue to lead an independent and fulfilling life while receiving one-on-one care for their dementia. It can also provides greater consistency than domiciliary care, where carers are likely to vary from day to day.
Of course, if you’re arranging care for a loved one, involving them in the process, if they have the capacity to voice their wishes is important. It may help to think about daily life together – ask them what care tasks they’d be comfortable with, and what areas of life could be made easier with a bit of outside help. Think about the benefits of care in relation to their lifestyle and what’s important to them. The following questions may help –
- Are you able to look after your home? What chores do you dislike or find most difficult?
- What hobbies and interests would be easier or more enjoyable with another person here?
- What local shops or places would you like to visit more if you could?
- Are there any friends and family you’d like to see more frequently?
- What meals or foods do you enjoy but find it difficult to prepare?
- Would you like someone to take the pressure off keeping appointments or managing post and paperwork?
For further dementia support, there are a number of other resources available, including –
- Admiral Nursing Dementia Helpline
- The Dementia Support Line from the Alzheimer’s Society
- Talking Point from the Alzheimer’s Society
- Reading Well
Tommy Dunne – Living with dementia, not suffering from it
Campaigner Tommy Dunne was diagnosed with Alzheimer’s at the age of 58 and now spends much of his time working with organisations such as SURF (Service Users Reference Forum), Liverpool Dementia National Alliance and YoungDementia UK to raise awareness of the issues around dementia. We talked to Tommy about how important is it for those with dementia to realise that they can still contribute to society and make a real difference.Read more care guides

The power of complementary therapies in dementia care
The power of complementary therapies in dementia care Alternative therapies might help a person manage some of the symptoms of dementia – these might be

Dealing with a dementia diagnosis
Dealing with a dementia diagnosis When your elderly loved one has just been diagnosed with dementia, they are likely to be overwhelmed by a range

Creating a dementia-friendly home environment
Creating a dementia friendly home environment Jump to Lighting Floors Furniture Technology Noise levels Outdoor spaces Bedroom Kitchen Bathroom Living with dementia can be

What is a memory clinic?
Memory clinic: What is it? Memory clinics are specialist centres that are often used to diagnose dementia. It’s somewhere you’ll usually be referred to after

What is an advance statement?
What is an advance statement? An advance statement is a written or verbal document expressing your loved one’s wishes when they no longer have the

Dementia care: Managing chewing and swallowing difficulties
Dementia care: Managing chewing and swallowing difficulties Caring for someone with dementia can be challenging at times, with different problems occurring as the disease progresses.
Read more care guides

How to prepare for a live-in caregiver
Care at home: how to prepare the home for a live-in caregiver A live-in carer can make a massive difference to your loved one’s quality

6 tips for finding the right live-in carer
Finding the right live-in carer is a significant and deeply personal decision, impacting your loved one and the entire family. You’re seeking someone trustworthy, compassionate,

The cost of care – everything you need to know
The true cost of care – everything you need to know Discover the true cost of care and explore your funding options with our care

Understanding autism in older adults
While Autism is usually diagnosed in childhood, an increasing number of older adults are being formally diagnosed in later life. Masking autism symptoms can result

A guide to speaking with a loved one about home care
Why do older adults resist care? A guide to speaking with a loved one about home care Bringing up the topic of care at home

How to choose the right personal alarm for seniors: A comprehensive guide
Personal alarms for elderly Discover how personal alarms work, who they’re best suited to, and how they provide greater peace of mind to older people