NHS Continuing Healthcare – your complete guide
NHS Continuing Healthcare covers every penny of your care costs. It’s available for anyone with long-term health needs. But many people don’t apply because they simply don’t realise it exists or assume they’re ineligible. However, you should never be put off.
NHS Continuing Healthcare (CHC) is a fully funded package of care that some people can claim due to a disability, accident or illness.
The application for NHS Continuing Healthcare is split into six stages. We’ll go into some of these in more detail later on, but for now, here’s a quick overview.
1) The initial screening assessment, or ‘the checklist’
This will work out whether your care needs qualify you for the full assessment. A health or social care professional will look at 11 areas of your health. If you have extremely severe needs, your application will be fast-tracked.
94% of those who have their application fast-tracked go on to receive funding
2) The full assessment and the decision support tool
This is an assessment designed to help your local Integrated Care Board (ICB) work out whether you’ve got a ‘primary health need.’
An assessment team will use a national framework called the ‘Decision Support Tool’ to score your needs and pass a recommendation of your eligibility to your ICB.
3) Receiving your decision
If you’ve been accepted for NHS Continuing Healthcare funding, a representative from your ICB will be in touch. They’ll book some time in with you to talk through your care needs. This will be your opportunity to make your preferences clear, for example whether you’d like to be cared for at home, or move into residential care.
4) Making an appeal
If you’ve not been accepted, but believe you should be receiving CHC, you don’t need to just accept the result of the assessment. There are often grounds for appeal. Writing to your ICB is the best place to start. We cover how to appeal a decision below.
5) Care planning
Your local ICB team will work with you to create your care and support plan. For more flexibility, you can take control of your funding with a Personal Health Budget – which can be paid directly into your account as a direct payment. If you’re arranging care with Elder, you’ll need to do this.
3) Review
Continuing Healthcare is not for life. You’ll have your circumstances reviewed to see whether the level of care is still suitable to support you and that you still have a ‘primary health need’. This will happen three months after being accepted and then annually after that.
What is Continuing Healthcare?
NHS Continuing Healthcare is care funding from the NHS for those with a primary health need.
Assessment isn’t based on any official diagnosis you’ve received. This means it doesn’t matter what condition you have. It doesn’t matter whether you’re in or out of hospital. It doesn’t matter about your financial means. And, it doesn’t matter whether you’re looking to pay care home fees, or for care at home.
If you get accepted, you won’t have to worry about care costs. And even if you don’t – getting your needs assessed by the NHS may help you get the local authority funding you deserve.
But what is it, how does it work, and how can you really maximise your chances of getting accepted? That’s what we’re about to talk through.
Who can get Continuing Healthcare?
Continuing Healthcare funds care for those with long-term, complex health issues. In the jargon, this is defined as someone with a ‘primary health need’ rather than a ‘primary social care need’.
This puts an emphasis on needs resulting from long-term health conditions, rather than needs resulting from getting older (such as frailty).
As you’ve probably noticed, this is quite a broad, subjective definition. Eligibility is actually worked out on a case-by-case basis.
It really boils down to the in-person assessment and the judgement of the team who are leading it. It isn’t linked to having a particular illness or condition.
It’s worth highlighting that while people do use NHS Continuing Healthcare to fund live-in care, CHC is reserved for those with more complex health and care needs. This often means those who qualify may require a level of care that falls outside of what an introductory service like Elder can provide.
What’s the difference between a primary health need’ and a ‘primary social care need?’
- Primary social care needs are when you need help to get on with your daily life. Think about your ability to: dress, eat, get around, look after your home, and maintain a social life.
- Primary health care needs are when your illness or condition means you need regular help. Think about these as support with breathing, understanding and awareness, risk of injury, help with medication and the general impact of the condition.
We cover the assessment in more detail later on. But this looks at a number of factors about your health to decide whether Continuing Healthcare is suitable. Largely, it looks at your needs and assesses the nature, intensity, complexity and unpredictability of them.
Ultimately, the best way to weigh up your likelihood of success is to think about how much care would be devoted to managing illnesses or conditions needs. Would your health get worse without the care?
That said, if you feel you’re in need of support, you should always apply for Continuing Healthcare.
Situations in which you could be assessed for Continuing Healthcare
If you’re in any of the following situations, you should be approached by a doctor or nurse to discuss your care and support needs:
- You’re being discharged from hospital – before you have gone through a local authority financial assessment.
- You’re going into residential care, with nursing support, without having received an NHS-Funded Nursing Care Assessment.
- Your mental or physical health has shown signs of significant decline, or if palliative care is being discussed.
Does dementia qualify you for NHS Continuing Healthcare?
Having a dementia diagnosis doesn’t mean you’ll qualify for Continuing Healthcare. As there isn’t a condition that automatically qualifies you for the funding.
If you have Alzheimer’s or any other form of dementia, it depends on the complexity, intensity and likelihood of your symptoms to be unpredictable.
If you don’t check, you’ll never know
If you’re living with dementia, don’t be put off applying. You won’t automatically qualify but are likely to still be eligible. Many people simply don’t apply.
Beyond simply personal care needs, those with dementia are more likely to get funding when their package of care requires frequent intervention.
Think about situations that lead to deep confusion, hallucination, sudden mood swings, disorientation – all which may put you or others at risk of harm.
How much is Continuing Healthcare funding?
There’s no cap on Continuing Healthcare – the NHS will simply pay for the care (and accommodation if needed) that you require – although this is assessed.
And, as it’s from the NHS, it’s universally free at the point of use. That means your finances make no difference to your eligibility.
This can be confusing when looking into care options for the first time. As you may have heard about a financial assessment or ‘means test’ when it comes to care funding. You may have also heard about asset thresholds, incomes assessments etc. This is only for local authority funding.
What is an Intergrated Care Board (ICB)?
In England, integrated care boards are regional NHS organisations responsible for planning and meeting the health needs of the people in it’s geographical area.
Think of them as your local council, but for NHS matters.
They lead the local strategy for planning how your local NHS hospitals, clinics and community health centres are run. Crucially, they’re also responsible for deciding whether you’re eligible for Continuing Healthcare funding.
Are these different from a Clinical Commissioning Group (CCG?)
ICBs were set up in July 2022 to replace clinical commissioning groups (or CCGs).
Another key area where Continuing Healthcare differs from local authority funding is that you’re unable to top it up. It should always cover your entire care costs, based on your individual needs.
There isn’t a cap on the amount you can receive. So, if you’ve been accepted for Continuing Healthcare but the sum you’re offered doesn’t meet your expectations, you should contact your ICB to explain why. Or, failing that, your Member of Parliament may be able to help you.
How do you apply for Continuing Healthcare?
To apply for Continuing Healthcare, you need to get in touch with a medical or social care professional who understands your needs. Who to contact depends whether you’re in hospital, or not in hospital.
Make sure you also speak directly with the NHS Continuing Healthcare team at your local ICB to get a clear understanding of the steps you need to take.
Don’t expect people to always know about Continuing Healthcare
Just because someone is in the NHS or social services, it doesn’t mean they know what Continuing Healthcare is. Actually, there’s quite a widespread lack of understanding about the funding stream. This may mean it’s not always presented to you as an option when, in reality, it should be.
It’s important you find someone who really understands the process. If your consultant isn’t able to help, visiting the Patient Advice and Liaison Services in your local hospital can be a great place to start.
If you’re in hospital
As we mentioned earlier, if you’re awaiting discharge from hospital and you have care needs, Continuing Healthcare should be discussed with you. If it isn’t, it’s time to be proactive.
- Speak to your ward consultant
- Ask whether they’re trained in Continuing Healthcare
- Begin the Checklist assessment
You may be tempted to ask a nurse or social worker. They may not be the best people to speak to. You’re usually best off speaking with your ward consultant. Find out when they’re doing their ward walkaround and approach them.
They’ll be able to advise you on what they think is best, and it’s always good to have a senior medical professional fighting your corner. If possible, ask them to complete the Checklist. If they don’t know about it, ask them to refer you to the Continuing Healthcare team. This group of specialists can help you with the first stage of the application.
If you’re not in hospital
The first thing to realise is that you’re still eligible. Many people are put off applying because they think you need to be awaiting discharge from hospital. This is not the case.
You should always apply to Continuing Healthcare before applying to local authority funding of you think you may be eligible – even if you’re not in hospital and even if you don’t have high hopes of success. If you’ve already gone to your local council or social worker, ask them about it.
Don’t be put off if they think you’re unsuitable – this is the job of the NHS assessors, not your local council. They should be able to help you contact your ICB’s local Continuing Healthcare team.
An alternative route is to start the process inside the health system. Your local GP or district nurse is a really great place to start, especially if they know you well. If they’re trained, they should be able to start your application with you.
If they’re not trained, they should still be able to refer you to the NHS Continuing Healthcare team, so you can begin the Checklist process. However, if they don’t know about the funding, you can search on the NHS website for local ICB.
- Speak to your GP or district nurse
- Get a referral to a local Continuing Healthcare team
- Start the application with the checklist assessment
What is the full application process?
There are several stages to getting Continuing Healthcare. It’s not a short process. It’s not a simple process. But don’t let that discourage you.
Take your time, do your research and be really clear on your care needs. Throughout the process, as the criteria are quite subjective, it’s ultimately down to the person assessing you. Which means it’s always worth applying.
What’s the difference between Continuing Healthcare and NHS-Funded Nursing Care?
NHS-Funded Nursing Care is a completely different funding stream to NHS Continuing Healthcare. Rather than paying for the full cost of your care, it covers only the nursing element of any care you receive.
It’s really important to ensure you apply for Continuing Healthcare first, and don’t accidentally end up applying for funded nursing care because of bad advice. This could result in you paying thousands of pounds in care fees that you could have had covered.
That said, if you find you’re not eligible for Continuing Healthcare, applying for NHS-Funded Nursing Care is often the next logical step. This can be worth £209.19 to be £287.78 per week, depending on your needs. A significant amount towards your total care costs.
Continuing Healthcare and other funding
It’s important to bear in mind that Continuing Healthcare can impact the state benefits you’re entitled to – depending on your circumstances. The main factor to consider here is where you’re receiving care.
What can NHS Continuing Healthcare be claimed with?
| Funding stream | Care home | Care at home |
| Local authority care funding | No | No |
| NHS-Funded Nursing Care | No | No |
| Attendance Allowance | No | Yes |
| Disability Living Allowance | No | Yes |
| Pension Credits | Some | All |
| State Pension | Yes | Yes |
How does Continuing Healthcare impact other benefits?
How does Continuing Healthcare impact Attendance Allowance?
It depends on where you end up receiving care. If you receive care in your own home, you’ll still be entitled to claim Attendance Allowance – provided you meet the criteria.
If you move to a care or nursing home, this will stop 28 days after you start receiving Continuing Healthcare.
Attendance Allowance is available for those who struggle to live independently without support. It’s aimed at people with a disability. You should always check whether you’re entitled to it, as it could provide you with additional income. This ranges from £68.10 per week to £101.75 per week.
How does Continuing Healthcare impact Disability Living Allowance?
Disability Living Allowance will not be affected if you’re receiving care at home. But, like Attendance Allowance, it will stop after 28 days if you go into a care or nursing home, unless you aren’t receiving care from a registered nurse.
However, in this case, it’s likely you may still continue to receive some disability funding. The mobility component of Pension Credit – the part of the benefit provided to fund mobility aids – will still be paid. You’ll be able to use this for ‘Motability’ transport – such as a mobility scooter.
How does Continuing Healthcare impact your State Pension?
Your State Pension is not impacted when you have your care funded through Continuing Healthcare.
But, if you stop receiving either Attendance Allowance or Disability Living Allowance, you will lose the ‘severe disability’ component of your Pension Credit.
As mentioned above, you’ll only lose these if you’re receiving care in a care or nursing home. The ‘severe disability’ component of your Pension Credit is worth £76.40 per week.
The 6 step guidance on CHC we go through on this page is specific to England only. This is because CHC works differently in Wales and has been replaced by an alternative initiative in Scotland.
Wales
To be eligible for CHC in Wales your local health board (LHB) will need to confirm that you have a primary health need. If you do, receiving CHC is your right.
There are seven LHBs to cover the Welsh regions.
The Welsh Government has created their own framework for implementing CHC in Wales. Unlike in the NHS England guidance, this framework states that CHC in Wales doesn’t cover all of a person’s care costs in full – but may cover most of them. For example, if you’re found eligible, the NHS will pay for things like personal care (help with washing, dressing, toileting) but are unlikely to cover things like housekeeping, support with cooking, running errands, or companionship.
This means that if you’re receiving CHC in Wales, it may not cover the full cost of something like live-in care.
You can read the Welsh Government’s guide on CHC here, or download their full framework here.
Scotland
In 2015 NHS CHC was replaced in Scotland with Hospital Based Complex Clinical Care.
Under this initiative, people are assessed for on-going care with one key question – ‘can your care needs be properly met in any setting other than a hospital?’
If they can, the local authority will take over to help arrange care in either a person’s own home, a care home, or supported accommodation. They’ll conduct a financial assessment and apply their funding and fees where applicable.
However, if a person’s needs cannot be met anywhere but in a hospital setting, their entire care will be funded by the NHS.
Read more about Hospital Based Complex Care here.
- Who is eligible for an NHS Continuing Healthcare Checklist?
- Who isn’t eligible for an NHS Continuing Healthcare Checklist?
- What’s your role in arranging a Checklist?
- What are the criteria in the NHS Continuing Healthcare Checklist assessment?
- What are the care domains in the NHS Continuing Healthcare Checklist?
- Who completes the NHS Continuing Healthcare Checklist?
- What are the outcomes of the Checklist assessment for NHS Continuing Healthcare?
- Tips for passing the NHS Continuing Healthcare Checklist
What is the NHS Continuing Healthcare Checklist?
The NHS Continuing Healthcare Checklist is the first stage of the assessment process. It’s a quick way for medical or social care workers to decide whether your application should be progressed to a full assessment. It’s an 11 point Checklist that looks into various care ‘domains’. These are essentially areas of your life you might need a bit of extra support with. We run through them in more detail below – but think about things like mobility, your mental health and how easily you’re able to breathe. Usually, it should be relatively quick to go through it, as it’s essentially pre-screening for the next stage in the process. The threshold for progressing through the Checklist is deliberately low – you’re likely to go through to the full assessment.Who is eligible for an NHS Continuing Healthcare Checklist?
- When you’re ready for discharge from hospital, prior to applying for local authority funding.
- If you’re going into a nursing home or care home, before you’re assessed for NHS-Funded Nursing Care.
- If your health – both mental or physical – is shown to be in rapid decline.
Live in a care home?
If you’re already in a care home, but you’re funding your own care, you could still be entitled to complete a Checklist. It could enable you to get care in your own home, if this is an option you’d prefer.Who isn’t eligible for an NHS Continuing Healthcare Checklist?
There are also certain grounds on which you can be rejected for a Checklist. The National Framework for NHS Continuing Healthcare Funding spells out the situations in which it’s considered unnecessary to complete the Checklist. They are:It’s obvious you’ll progress
If it’s extremely obvious to the health or social care professional looking at your needs that you’ll pass, they can forward you to the full assessment. This means a Checklist is simply not needed.It’s obvious you’ll not progress
If it’s clear to your GP, district nurse, social worker, or other health and social care worker that you don’t have a ‘primary health need’ they may decide there is no need for you to take it. However, if there is doubt between practitioners – for example, your social worker thinks you should take it and your GP doesn’t – you should be permitted to undergo it.Appointing a loved one to act on your behalf
If you’re fast-tracked
If you have a “rapidly deteriorating condition that may be entering a terminal phase”, you’ll be fast-tracked through the assessment process. This means you’ll go straight to the full assessment. Usually you can begin receiving funding within 48 hours.If your needs are still not clear
The Checklist should be taken when the long-term implications for your health become more apparent. If it’s deemed your health needs are currently just short-term, they may not progress you to a Checklist. However, you should always push for them to do the initial assessment if you think there’s any doubt.What’s your role in arranging a Checklist?
It’s really essential you – or a nominated family member – are fully involved in the process. This means you should be informed when, where and by whom the Checklist is being performed. It’s not uncommon for this not to happen – and people simply being informed of the outcome. This is often because health and social care professionals aren’t fully aware of the principles of the National Framework for Continuing Healthcare.A report by the Continuing Healthcare Alliance found that around 60% of healthcare professionals are assessing people without sufficient specialist knowledge of the medical condition that they are looking at. House of Commons, Public Accounts Committee, 2018You should always be made aware of when the Checklist is taking place, and it should only be done with your consent. If mental capacity means you’re unable to consent, you’ll need someone with legal permission to do so. This has to be someone with either Lasting Power of Attorney or someone who has been appointed as your Personal Welfare Deputy. If you find a Checklist has been completed without your knowledge, you should challenge it. And, if necessary, ask for it to be taken again.
What are the criteria in the NHS Continuing Healthcare Checklist assessment?
The Checklist is a screening tool to look at your eligibility for a full assessment. It looks at 11 ‘care domains’. For each of the ‘domains’, you can be marked with a score of A-C, with A being the most severe.- You’ve scored A in two or more domains.
- You’ve scored B – or one A and four Bs in five or more domains.
- You’ve scored an A in any of the four ‘priority domains’.
What are the care domains in the NHS Continuing Healthcare Checklist?
A ‘care domain’ is an area of your health and wellbeing where you may need to support. There are 11 in total, including four priority domains: ‘Behaviour’, ‘Breathing’, ‘Medication’, and ‘Altered State of Consciousness’. Scores in these areas count more than in others.- Behaviour*
- Cognition
- Psychological or emotional
- Communication
- Mobility
- Nutrition
- Continence
- Skin integrity
- Breathing*
- Medication*
- Altered state of consciousness*
Behaviour*
Behaviour is a priority domain which means it counts more towards the threshold for eligibility. The main criteria the assessor is looking for is whether they consider your behaviour to be ‘challenging’. Challenging behaviour includes aggressive violent or non-violent actions, extreme mood swings, persistent restlessness, self-harm, destructiveness, disruptiveness, or inappropriate sexual behaviour. Like everything else in NHS Continuing Healthcare assessments, what defines ‘challenging behaviour’ remains somewhat open to the interpretation of the assessor. The information in the following tables for each domain are summaries, and not complete lists. You can view the full Checklist here.| C | B | A |
|---|---|---|
| Little evidence of ‘challenging behaviour’ that poses a risk to yourself or others. Or no challenging behaviour at all. | Predictable ‘challenging behaviour’ that a social care professional is able to manage, that doesn’t pose a risk to yourself or others. | Challenging behaviour’ poses a risk to yourself or others. In this scenario, it can be difficult for even a professional carer to support you. |
Cognition
This looks at how you’re practically able to process thoughts and feelings – and the impact not being able to do so has on your daily life. The assessor will look at your general cognitive state. This includes your level of disorientation, levels of confusion and memory. As well as your ability to make decisions. Practically, assessing your cognition will look at how much support you need to minimise the risk of harm. Before completing the Checklist, it can help to discuss your memory during day-to-day living with a loved one. If you’re able to provide practical examples, this will always help the assessor.| C | B | A |
|---|---|---|
| You need some assistance with more complex tasks, e.g. managing finances or occasional issues with memory and decision making. Or no issue with cognition at all. | Memory issues mean you require some support to make decisions. Your general inability to make decisions puts you at some risk of harm. | Limited awareness of only basic tasks. You’re unable to make decisions on key aspects of your life without supervision. You’re at risk of harm without support. |
Psychological or emotional
Typically a really important domain for those living with dementia, the psychological and emotional domain looks at how your mood and psychological condition are impacting your wellbeing. The assessor will talk through any issues such as anxiety, depression or withdrawal from your daily activities. They’ll also consider whether these issues have come to light because you’ve not engaged in care planning previously. If you’ve found it difficult to accept help from others, it’s more difficult for you to recover.| C | B | A |
|---|---|---|
| Anxiety or changes in your mood are impacting your life but you’re responding to reassurance. You might require a bit of emotional support, or none. | You’re not responding well to reassurance and anxiety or distress are increasingly impacting your wellbeing. This may result in you withdrawing from daily activities. | Your mood has a severe impact on your daily life. Your psychological or emotional state means you withdraw from the offer of support and normal activities. |
Communication
| C | B | A |
|---|---|---|
| You’re able to communicate clearly – whether spoken or unspoken. Or, it might take someone a bit of effort to get an accurate idea of what you’re trying to get across. | It’s tricky for you to communicate about your needs, even with support. You probably rely on non-verbal signalling, or your carer has had to grow accustomed to how you communicate. | The majority of your needs are anticipated by your carer, as you’re not really able to communicate effectively. Or you’re unable to communicate at all. |
Mobility
| C | B | A |
|---|---|---|
| You’re completely independently mobile or require some equipment to support you with daily living – such as a walking stick. | You’re wobbly on your feet, not able to consistently bear weight, you don’t move for long periods, or you’re deemed to be at risk of a fall. | You’re unable to bear weight, are in significant pain while moving, have lost muscle, or are deemed to be at a high risk of a fall. |
Nutrition
Nutrition focuses on how easy you find it to eat or drink. The assessor will consider your risk of not eating enough food (malnutrition) or not drinking enough water (dehydration). For those who have survived a stroke, in the late stages of dementia, or are living with Parkinson’s – this can be an important domain. Nutrition also looks at weight loss or gain. So if you’ve seen big changes in your weight, this will be taken into account.| C | B | A |
|---|---|---|
| You’re able to independently eat or drink, or you need a bit of support – with feeding or supervision. You may have a pureed diet. | It takes you a long time to eat – even if the food is pureed, or you’re not able to eat or drink by your mouth and require a PEG. | You have real difficulty swallowing to the extent it presents a risk, you’re having problems with PEG feeding, or you’ve shown big changes in weight. |
What is PEG feeding?
Continence
Continence focuses on how you’re managing with going to the toilet. This can range from those who are completely in control of toileting to those who have constant difficulties. For example, aren’t able to know when they need to go, or are unable to control it when they do. You might be surprised to know that being double incontinent – where you have little or no control over going for a poo or a wee – is not considered high needs. That’s because this is considered to be a social care need. For a ‘primary health need’, the assessor will consider how your incontinence has the potential to impact your health – looking at the likelihood of illness or infection. A common example of this would be a urinary tract infection (UTI).| C | B | A |
|---|---|---|
| You don’t have any issues that aren’t able to be managed through medication or regular toilet trips, you’re using a stoma without any issues, or you only have occasional issues. | Your continence needs require monitoring, you’re doubly incontinent, you have common urinary tract infections, or you use catheters that need replacing occasionally. | You need regular specialist support to ensure your continence issues don’t put you at risk. This is beyond routine hygiene – e.g. bladder washing or replacing catheters frequently. |
Skin integrity
Skin integrity looks at the health of your skin, and the risks associated with poor condition. This will look at how fragile your skin is – for example how easily it can be pierced or irritated. This is closely linked to mobility because if you’re spending a lot of time in bed, that puts you at a higher risk of conditions such as bed sores or skin ulcers. The assessor will consider how much treatment your skin needs on a daily basis to minimise ongoing risks.| C | B | A |
|---|---|---|
| You don’t have any damage to your skin, you require daily treatment to prevent skin damage, have minor pressure damage – such as an ulcer, or you have a specific skin condition. | You require treatment to prevent damage a few times a day, you have damage to your skin – such as pressure ulcers, you have a skin condition that requires daily treatment. | You have open wounds that aren’t responding to treatment, you have a severe loss of skin thickness – making wounds more likely, or you’re requiring daily skin dressings. |
Breathing*
| C | B | A |
|---|---|---|
| You’re not having any issues with your breathing, you have shortness of breath and your inhaler works, or you’re able to manage periods of breathlessness. | You have shortness of breath that impacts some daily activities, some shortness of breath can’t be managed, you require advanced support with breathing – such as room air ventilation. | You’re only able to breathe independently through a tracheotomy, your breathing has a severe impact on your daily life, or you require a non-invasive ventilator. |
What is a tracheotomy?
Medication*
Medication and symptom control is a priority domain that looks at the complexity of the prescriptions you have to take, and considers the impact of not taking them – or not taking safely – upon your health. It also looks at the equipment and human support you need to manage symptoms and minimise risk. At a basic level, you may need someone to remind you to take your medication. But, with acute needs, you may need constant monitoring to ensure you’re getting the right dosage. Have a think about times in which you’ve not understood what medication you need to take, have missed vital medication or have even risked overdosing.| C | B | A |
|---|---|---|
| You don’t take medication, or you do and it has few side effects and you’re complying with prompting to take your medicine. You may feel mild pain when performing strenuous activities. | You need support to help administer your medication, there is a big risk to you not taking it, or it’s complex to take. You might feel moderate pain with certain activities. | You need intensive monitoring and support of health or social care workers to ensure medication is taken or applied sufficiently. You have moderate to severe pain, impacting other care domains. |
Altered state of consciousness*
| C | B | A |
|---|---|---|
| You aren’t experiencing any episodes of altered consciousness or you have in the past, but there’s little risk today. | You experience episodes of altered consciousness monthly and need a carer to support you when they occur. | You experience episodes of altered consciousness regularly and need a carer to constantly support you. |
Who completes the NHS Continuing Healthcare Checklist?
Get someone you know and trust to perform the Checklist
What are the outcomes of the Checklist assessment for NHS Continuing Healthcare?
There are three main outcomes of the Checklist assessment. You can be:- Accepted to the full assessment
- Not put through to the full assessment
- Fast-tracked, if you have urgent or palliative needs
How many people pass the NHS Continuing Healthcare Checklist?
Positive outcome
Passing the Checklist doesn’t mean you’re entitled to NHS Continuing Healthcare funding. It means you go forward to the next stage – the full assessment of eligibility. We’ll go on to talk about this in more detail later. However, the full assessment is undertaken by a multidisciplinary team of health and social care professionals.Negative outcome
If you don’t meet the criteria, you’ll not be passed through to the full assessment. You should receive written confirmation of your Checklist results. If you don’t receive these, it’s important you reach out to the health or social care professional who has performed your Checklist assessment. If you’re not put forward to the full assessment, all hope is not lost. You have 12 months to appeal the decision. To do this, you should write to the NHS Continuing Healthcare team at your local Integrated Care Board. Along with a letter of appeal, you should include any additional evidence you have that supports the idea you have a primary health need. This is where keeping a diary of how your illness or condition impacts your daily life will really pay off.How do you appeal a negative Checklist outcome?
- Write to your ICB, explaining why you think the outcome is wrong.
- Include evidence that shows you have ongoing health needs.
- Request that another Checklist assessment is carried out.
- If the outcome is again negative and you still believe this to be wrong, you have the right to begin the NHS complaint procedure. You can submit a written complaint to the ICB Complaint Manager, and forward it on to the Parliamentary and Health Service Ombudsman.
The Fast Track Pathway outcome
The Fast Track Pathway is there in case your needs are urgent or getting worse quickly. A clinician – so a doctor or nurse – who has a thorough knowledge of your situation can instantly refer you for funding. This decision is taken if you’re in a situation where every moment you have left really counts. It’s a far simpler process, that requires your ICB to approve and arrange funding as quickly as possible. This is meant to be put in place within 48 hours, but research by Marie Curie has indicated that around a third of people have to wait longer than a week. Many people, including health and social care professionals, think this is just for end of life support. However, this is not the case. If you are entering the terminal phase of your life, and your situation is getting increasingly difficult very quickly, you should always push for Fast Track funding. Fast track assessments are almost always approved. Looking at the NHS report for 2021-2022, of the 23,823 fast track assessments completed – every single one was successful.Tips for passing the NHS Continuing Healthcare Checklist
Tip one: Always do the Checklist
It doesn’t matter whether you or your healthcare professional think there’s little chance you’ll be accepted. The Checklist is a screening tool. It’s purpose is to help decide whether your situation is right for the full assessment. It can be easy to accept a recommendation to not bother completing the Checklist – especially if it’s a healthcare professional you trust. But it’s important to resist the temptation. Even if you feel you’re being difficult, you should insist on taking the Checklist.NHS continuing healthcare (CHC) funding is intended to help some of the most vulnerable people in society but too often people’s care is compromised because no one makes them aware of the funding available, or helps them to navigate the hugely complicated process for accessing funding. House of Commons, Public Accounts Committee, 2018
Tip two: Always be there when it’s done
You should be fully informed about where, when and by whom your Checklist is being completed. There’s no better way of staying informed than being there in person. This will usually happen as a matter of course, However, if it doesn’t, you really should be insistent. Being there means you’re able to provide practical examples of how each care domain has an impact on your life. This could make it much more likely for your application to be progressed. Even if you’re unable to go yourself, you should make sure that a nominated person goes in your place.Tip three: Ensure relevant training
A variety of health or social care professionals are able to run the Checklist assessment. However, they should always have been trained in the tool. That’s the essential requirement. Before you undertake the Checklist, be sure to make a note of the time, date, location, and name of the professional who’s undertaking your test. It’s not rude to ask them whether they’ve been trained in the tool – it’s your right.Tip four: Complete it anywhere
It’s crucial to understand that not everyone working for the NHS will have an understanding of Continuing Healthcare funding. This may lead to you receiving information that isn’t always accurate. A classic example of this is being told the Checklist must be completed in a care home, or in a hospital. Although these are two common locations, you’re actually able to have this initial assessment done wherever is best for you. For example, it can be completed in your own home.Tip five: Be persistent, not pushy
If you’re fully informed of the process – and your rights, you should have confidence in your knowledge. There are many in the health and social care sector who unfortunately lack full knowledge of Continuing Healthcare. This can impact your Checklist results. You should always pick professionals up on the following:- Not considering your needs against moderate and high needs – only looking at the ‘C’ criteria.
- Your ICB don’t accept the findings of the health and social care worker. But there’s no obvious reason given.
- Not considering you for a Fast Track Pathway, when you feel you’re suitable.
- The changing nature of your needs wasn’t considered. They only looked at how things are today, not how things will be in the near future if you don’t get support.
- How to get a Continuing Healthcare assessment?
- Who carries out the NHS Continuing Healthcare assessment?
- What happens at the multidisciplinary team assessment?
- What should you say at your NHS Continuing Healthcare assessment?
- Tips for a successful Continuing Healthcare assessment
What is the Continuing Healthcare assessment?
The assessment is the second and final stage in the assessment process for Continuing Healthcare. It’s a detailed review of your care and support needs performed by a multidisciplinary team. If you meet the criteria, your ICB will arrange all of your care homes fees, or fees for support in your home to be covered. An assessment is automatically booked once you’ve passed the initial screening “Checklist” stage. Working with social care professionals from your local authority, a team from across health services will talk through your personal care needs. They’ll judge your need for a package of care based on something called the Decision Support Tool. The outcome isn’t determined immediately after the assessment. The information is passed on to your ICB. They’ll then get back to you with their decision – this should be within 28 days.Be prepared –the wait may be longer
A 2021 – 2022 report by NHS England revealed that 1,774 people waited longer than 28 days for their assessment to be completed. 284 of these people waited up to 26 weeks.How to get a Continuing Healthcare assessment?
You can get a Continuing Healthcare assessment only after completing the Checklist stage. We run through this in the previous section. As we’ve covered, anyone can apply for this – provided there’s a realistic chance they have a ‘primary health need’. After you’ve passed the Checklist, your local NHS should automatically refer you to a full assessment. Under the National Framework – the rules that guide Continuing Healthcare – this should be within 28 days of your Checklist.What should you do if there’s a delay in arranging an assessment?
Unfortunately, the reality is it usually takes longer than the stated time period as we’ve shared above. Beacon, a charity specialising in assisting people with their Continuing Healthcare claims, estimates that only 5% of assessments are on time. If you’re deemed eligible, your funding will be back-dated to the date you were referred to the full assessment. This is frustrating. If your needs are urgent, you can write to your ICB and ask them to reconsider you for the Fast-Track pathway. If your full assessment is facing delay – you should raise this with your Coordinating Assessor. You’ll be given their contact details when you’re referred to the assessment. Ask them for clarification on why the delay is occurring. It’s important to be insistent, reminding them of their duty of assessment within 28 days under the National Framework. Then, if you’re still not happy with the timescales they’ve given – you should complain to your ICB using the NHS Complaints Procedure. If your needs are more long-term and a few extra weeks make little difference, you can use this time as an opportunity to prepare yourself for the full assessment. Giving yourself the best possible chance of being accepted.How to use delays to your advantage
- Keep a diary of the way in which your health needs are impacting your day-to-day life.
- Look for the Decision Support Tool by searching online, and score yourself against it. This will give you a good idea of what you think you’ll be entitled to.
- Talk with your social worker and any healthcare professionals working with you. Ask them for their views on potential weaknesses in your case – and prepare a counter-argument.
Who carries out the NHS Continuing Healthcare assessment?
Your main assessment for Continuing Healthcare should be completed by a multidisciplinary team of different health and social care professionals. They work together to ‘collate and review’ all the important information that relates to your health needs. Before completing the Decision Support Tool, and passing on a recommendation to your ICB. They’re the body ultimately making the decision about your eligibility.- The team assessing your needs should have at least one person from a healthcare background and one person from a social care background who are both familiar with your case.
- Generally, it’s best that more than two professionals attend. If you have one, you should request your social worker to be present – especially if you have a good relationship with them.
- There should always be someone present from your local authority. Ultimately, your ICB will have to consult your local council before coming to a conclusion on whether or not you’re entitled to Continuing Healthcare. If there’s nobody at the assessment representing the local authority, this won’t be possible. That means the assessment will not be valid.
- Everyone in the team should be trained in the NHS National Framework on Continuing Healthcare. If they’re not and you find you’re not accepted, this will be grounds for appeal.
- It’s best practice to have specialists present if you have specific areas of difficulty, for example, it’s best to have a speech therapist or sign language interpreter available if you’re struggling to communicate. Someone who can help you get your voice heard. This is critical – as your opinion is an essential part of the evidence used to consider your eligibility.
What is a Coordinating Assessor in Continuing Healthcare funding?
The Coordinating Assessor is the representative from your ICB who is the case manager for your application. They’ll be responsible for bringing together the multidisciplinary team, who’ll complete the assessment. They’re also the person who should make sure you’re properly involved at every stage of the assessment. If you feel you’re out of the conversation, you should get in touch with them. If you feel they’re not sufficiently knowledgeable in Continuing Healthcare, you should contact your ICB directly.What happens at the multidisciplinary team assessment?
At the multidisciplinary team assessment, the team will look through all the relevant evidence around your health and care needs. It should be a thorough discussion that talks through each of the ‘care domains’. These are the same 11 domains we mentioned at the Checklist stage. However, this time there’s an additional, more open domain called ‘other specific care needs’. This means the team will look at 12 domains in total. If you’ve already had a care needs assessment from your local authority, this will be an important piece of evidence. But they’ll also consider medical records, the view of your social worker and any material you’ve submitted – such as a diary or photographs. Remember, it’s also really critical they ask you about your own preferences. What you want to happen is not a side note. It’s of central importance to getting the right outcome.What should not be considered at the assessment stage?
There are certain areas that should not be taken into consideration when you’re being assessed. If they are, you should feel confident in being vocal. Gently remind the team that it’s out of scope.- your assets
- your income
- diagnosis for a particular condition
- where care is being, or will be, given
- a specific provider’s ability to manage your needs
- specialist staff being present in care delivery
- how your needs are currently managed
- that you’re receiving NHS-funded Nursing Care
- anything that doesn’t relate to your care needs
What should you say at your NHS Continuing Healthcare assessment?
The most important thing to get across is how you feel about the situation. You should think about the following questions:- How is your health impacting the way you live your life?
- How often do you need the support of someone else?
- What would be your ideal care package?
Tips for a successful Continuing Healthcare assessment
Ahead of your assessment, it’s important you prepare yourself. The more information you have about the process – and the more confidence you have in understanding your needs, the more likely you are to be successful.Tip one: Score yourself using the Decision Support Tool
You should make sure you’ve got a really good understanding of the Decision Support Tool. That’s not just about research – which is probably why you’re on this page. It’s about generating a real understanding of the way in which your needs fit into the framework. There’s no better way of doing this than assessing your needs against the tool. You can find a copy of the tool here. Have a go at going through it yourself. What score would you give your needs? Where do you think you need the most support?Tip two: Keep a record of your care journey
At every stage, you should make sure you’ve made a note of every interaction you’ve had with those involved in Continuing Healthcare. If there are any moments that stand out, make sure you have your own side of events in case your assessment is rejected.Tip three: Be there for the assessment
Like the Checklist, it’s essential that you go to the assessment. If you don’t, your voice simply will not be heard. As we’ve said, nobody understands your situation better than you do. The assessors can’t build the complete picture of your life without you being there. Proactive research into the rules, followed by solid preparation for expected questions in the key care domains is critical to success. But only if you’re there to defend yourself in the flesh. If you’re unable to be there, make sure a loved one can.Tip four: Get to the assessment ahead of time
Ensure you arrive at your assessment with plenty of time. This may sound like an obvious thing to say. But it’s really important. There have historically been reports of assessments being completed early – before the person being assessed arrives. Obviously, this is completely unacceptable. But it can be avoided with good timekeeping.Tip five: Discuss things with your social worker
Your social worker is on your side. Before your assessment you should speak with them about the questions they expect to come up. You should ask them which care domains they feel you should focus on. You should also get an idea of how hopeful they are about your chances of success. Ultimately, it pays to build a good relationship with your social worker. They’re likely to be one of the assessors.- How is your health impacting the way you live your life?
- How often do you need the support of someone else?
- What would be your ideal care package?
Tips for a successful Continuing Healthcare assessment
Ahead of your assessment, it’s important you prepare yourself. The more information you have about the process – and the more confidence you have in understanding your needs, the more likely you are to be successful.Tip one: Score yourself using the Decision Support Tool
You should make sure you’ve got a really good understanding of the Decision Support Tool. That’s not just about research – which is probably why you’re on this page. It’s about generating a real understanding of the way in which your needs fit into the framework. There’s no better way of doing this than assessing your needs against the tool. You can find a copy of the tool here. Have a go at going through it yourself. What score would you give your needs? Where do you think you need the most support?Tip two: Keep a record of your care journey
At every stage, you should make sure you’ve made a note of every interaction you’ve had with those involved in Continuing Healthcare. If there are any moments that stand out, make sure you have your own side of events in case your assessment is rejected.Tip three: Be there for the assessment
Like the Checklist, it’s essential that you go to the assessment. If you don’t, your voice simply will not be heard. As we’ve said, nobody understands your situation better than you do. The assessors can’t build the complete picture of your life without you being there. Proactive research into the rules, followed by solid preparation for expected questions in the key care domains is critical to success. But only if you’re there to defend yourself in the flesh. If you’re unable to be there, make sure a loved one can.Tip four: Get to the assessment ahead of time
Ensure you arrive at your assessment with plenty of time. This may sound like an obvious thing to say. But it’s really important. There have historically been reports of assessments being completed early – before the person being assessed arrives. Obviously, this is completely unacceptable. But it can be avoided with good timekeeping.Tip five: Discuss things with your social worker
Your social worker is on your side. Before your assessment you should speak with them about the questions they expect to come up. You should ask them which care domains they feel you should focus on. You should also get an idea of how hopeful they are about your chances of success. Ultimately, it pays to build a good relationship with your social worker. They’re likely to be one of the assessors.- What are the levels of need?
- What level of need do you have to have to be eligible?
- What are the Decision Support Tool care domains?
- How do assessors use the Decision Support tool to judge your care needs?
What is the Decision Support Tool?
Think of the Decision Support Tool as a set of standards by which your needs will be judged. It’s usually completed by the multidisciplinary team after your assessment. As with the Checklist, it’s a way of providing a consistent assessment of your care needs. It cannot be completed without you having gone through the multidisciplinary team’s assessment. Importantly, it should be used as an aid. The National Framework says the Decision Support Tool is there ‘to facilitate consistent, evidence-based assessment’. The view of the assessor – based on the evidence provided during your assessment– is what’s ultimately important in terms of coming to a recommendation.What are the levels of need?
For each of the domains, your needs will be marked by a level of severity. These will inform the recommendation the assessors pass on to your ICB. They are:| No needs | Low needs | Moderate needs | High needs | Severe needs | Priority needs |
|---|---|---|---|---|---|
| You don’t have any evidence of issues in the area. | Your life isn’t being impacted and care is effective. | Your needs impact your life but are manageable and predictable. | Your needs are impacting your life, support isn’t always effective. | Your needs are frequent and may present a risk to you and others. | Immediate intervention is required, you need constant care. |
What are the levels of need?
What level of need do you have to have to be eligible?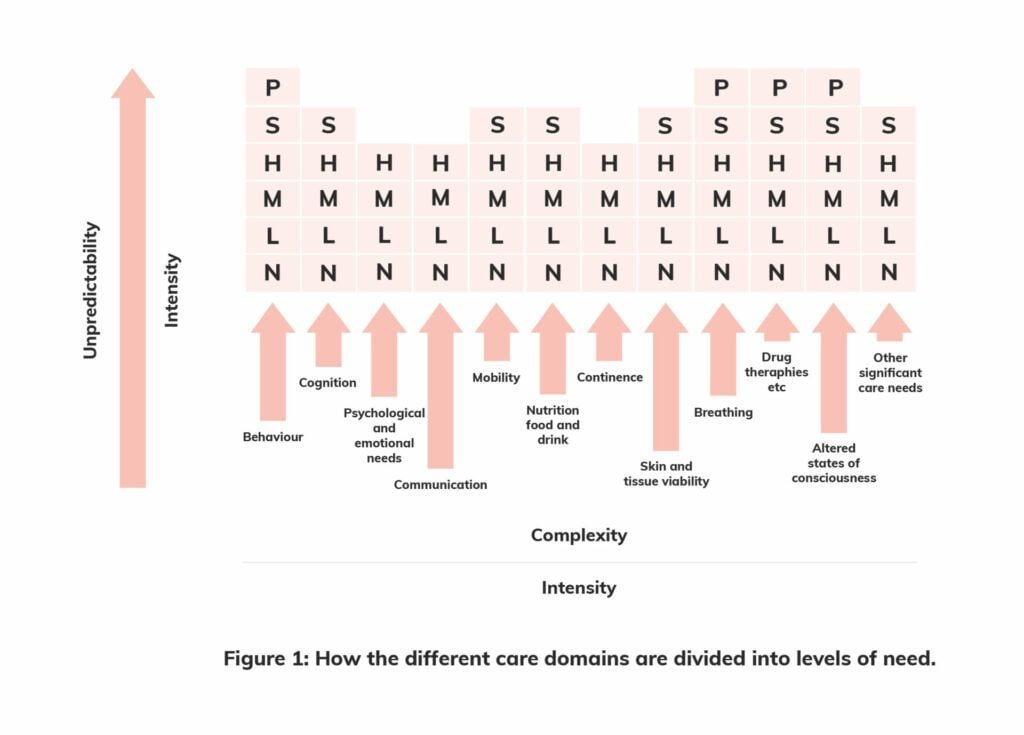 For a clear recommendation of eligibility you’ll need:
For a clear recommendation of eligibility you’ll need:
- A priority level of need in any of four ‘priority domains’, or
- Two or more ‘severe’ levels of need in any of the domains
- One domain recorded as ‘severe’ (S), with a number of ‘moderate’ needs and above in a number of other domains, or
- A large number of domains in which you have ‘high’ (H) and ‘moderate’ (M) needs.
What are the Decision Support Tool care domains?
In the previous chapter, we’ve covered the care domains in quite a lot of detail. So you’ve probably got a good idea of what they are. At the Decision Support Tool stage, there is also an additional domain, ‘other significant care needs’. It’s there in case some of your requirements don’t neatly fit into the 11 prescribed care domains. To get an idea of the specific requirements for a high-priority level of need of the following domains, take a look at the criteria of anything that scores an A at the Checklist assessment.- Breathing
- Nutrition
- Continence
- Skin integrity
- Mobility
- Communication
- Psychological & emotional needs
- Cognition
- Behaviour
- Medication
- Altered states of consciousness
- Other significant care needs
How do assessors use the Decision Support Tool to judge your care needs?
What’s important to understand is how each of the domains are assessed when someone is filling out the Decision Support Tool. The guidance notes for assessors asks them to consider specific questions around nature, complexity, intensity and unpredictability for each domain. They should also consider how these needs are likely to change in the future and discount how your needs are currently being met. Ahead of your assessment, you should prepare answers to these questions for each care domain – but especially those domains for which you received a higher score at the Checklist assessment:Nature
This looks at the specific detail of your needs and the type of support you require to live well with them. It’s important to put together responses for the following:- How does the individual or the practitioner describe the needs (rather than the medical condition leading to them)? What adjectives do they use?
- What is the impact of the need on overall health and well-being?
- What types of interventions are required to meet the need?
- Is there particular knowledge/skill/training required to anticipate and address the need? Could anyone do it without specific training?
- Is the individual’s condition deteriorating/improving?
- What would happen if these needs were not met in a timely way?
Intensity
This takes into consideration the number of health needs you have in each of the care domains and how severe each of these individual needs are. You should think about preparing answers for the following questions, for each care domain:- How severe is this need?
- How often is each intervention required?
- For how long is each intervention required?
- How many carers/care workers are required at any one time to meet the needs?
- Does the care relate to needs over several domains?
Complexity
The assessor will consider how much skill or equipment is needed as well as considering how you respond to support. As with the other characteristics, you should prepare answers for each of the domains for the questions assessors are guided to ask:- How difficult is it to manage the need(s)?
- How problematic is it to alleviate the needs and symptoms?
- Are the needs interrelated?
- Do they impact on each other to make the needs even more difficult to address?
- How much knowledge is required to address the need(s)?
- How much skill is required to address the need(s)?
- How does the individual’s response to their condition make it more difficult to provide appropriate support?
Unpredictability
This considers stability – how your needs change from one moment to next, what challenges this creates, and the level of risk to your health. Consider preparing answers to the following questions for each domain:- Is the individual or those who support him/her able to anticipate when the need(s) might arise?
- Does the level of need often change? Does the level of support often have to change at short notice?
- Is the condition unstable?
- What happens if the need isn’t addressed when it arises? How significant are the consequences?
- To what extent is professional knowledge/skill required to respond spontaneously and appropriately?
- What level of monitoring/review is required?
What happens after the NHS Continuing Healthcare Assessment?
After the team has completed the assessment and completed the Decision Support Tool, they’ll pass a recommendation about your eligibility to your ICB. Ultimately, it’s then up for the ICB team to decide whether or not you’re approved for Continuing Healthcare. You should hear back within 28 days. However, research by the Continuing Healthcare Alliance has found that as many as 42% of people wait longer for a result – with little or no communication. If this happens to you, you should contact your Continuing Healthcare team. Along with the decision of whether or not you’ve been approved, you’ll also be informed about the level of support available to you.Care and support planning
If you’re eligible, you’ll go into care and support planning. With the help of your assigned caseworker, usually a social worker or occupational therapist, this is the stage where you decide on the options that are best for you. For many, the extensive nature of their needs will mean a nursing home is the only realistic option. But, for a lot of people, this could mean you’re able to get care in your own home. At this point, it’s crucial that you’re vocal about what you think is best. Your ICB has to work with you in collaboration – appreciating your wishes. As with the assessment stage, the National Framework for Continuing Healthcare specifically states that you should be involved in decision making. To take control of your funding, you can request a Personal Health Budget.What is a personal health budget?
A personal health budget has been the default option for NHS Continuing Healthcare since April 2019. It’s when a monetary value is put on your NHS Continuing Healthcare entitlement. You then have a number of options around how you want this to be administered. For example, you can choose to take this as a direct payment, which puts you in control of the type of care you want to receive. This is often the best choice for those who have decided care in their own home is their favoured solution. The aim is to give people more control and choice around deciding what suits them best.Don’t take no for an answer
How is your personal health budget paid to you?
There are three main ways your personal health budget can be spent. And, most of the time, it’ll be up to you to decide on what you think is best for your situation.| A direct payment | A notional budget | A third party arrangement |
|---|---|---|
| You take control over the management of your plan, and simply have to keep evidence to show you’ve spent the money on care. | You’re still able to have significant input into the type of care you go with, but the NHS will arrange it for you. They’ll pick the care provider. | A third party, such as a trust, controls the money and manages your care and budget, in accordance with your agreed care plan. |
Appealing a decision if you’re not eligible
Getting turned down for Continuing Healthcare can feel daunting and occasionally upsetting. However, there are always next steps. The first step is to appeal, then it’s time to look at other funding options. Along with the decision not to progress your Continuing Healthcare, your local ICB should provide you with information on how to appeal – as well as the reports from the Decision Support Tool or Checklist assessment. You’ll have six months from the initial decision to request a review. Here’s how the appeals process works:1. Write to your local ICB
2. Provide evidence to support your claim
3. Appeal review and reassessment
4. Request an independent review
5. Write to your local MP
Getting NHS-Funded Nursing Care
If you’re not eligible for Continuing Healthcare funding, that doesn’t mean you’re unable to get any funding from the NHS. NHS-Funded Nursing Care is when the health service pays for the nursing component of your care. This is anything that has to be delivered by a registered nurse. Tasks that a nurse has to perform include more complex tasks around monitoring or managing your condition, for example administering injections, or STOMA care. You’ll only be able to use NHS-funded Nursing Care if you’re in a residential home. But – as with Continuing Healthcare – your financial situation is not taken into account.How much is NHS-Funded nursing care?
NHS-Funded nursing care has two rates. It’s tax-free and doesn’t impact your other benefits.- The standard rate for NHS-Funded nursing is £209.19 per week.
- The higher rate – for those with more acute needs – is £287.78 per week.





