What is the osteoporosis T-score?
As our bones grow they increase in density – usually reaching maximum density in our twenties. This density then begins to decrease as we get older. Lower bone density can leave them more fragile and prone to breaks. In later life, a person may be referred to a specialist to check their bone density through a bone density scan. This is a quick and painless procedure that will give your bones a score, and helps identify bone strength, and inform lifestyle changes to better care for and protect your bones.
What is a t-score?
A T-score is a standard deviation result of your bone density scan. A standard deviation result is usually based on a population standard or the average score of an entire population. In this case, standard deviation shows how much your bone mass differs from an average healthy adult of 30 years old.
A T-score for normal bone density is -1 and above. This means your bone mineral density is average. If your bone density measurements are between -1 and -2.5 your bone density is below average, and your doctors will call this Osteopenia. Osteopenia is the stage before osteoporosis when you have lower than average bone density for your age but not low enough to be classed as osteoporosis. Osteopenia does not always lead to osteoporosis, as there are ways to keep your bones healthy.
When your T-score is -2.5 and below, you’ll likely be diagnosed with osteoporosis because your bone density is too low, and you are at a higher risk of bone fracture.
How is the T-score test performed?
Your T-score is found using a DEXA scan, sometimes known as a Bone Density scan; this does not involve the need to go into a tunnel scanner like with an MRI, any injections or medications. Bone density testing using a DEXA scan(Bone density scan) involves lying flat on your back on an open x-ray table. During the scan, a large scanning arm passes over the body to get a measurement of bone density in the centre of your skeleton. You will need to be still during the exam so the images do not blur and the machine can make an accurate measure.
Usually, a narrow beam of low-dose X-rays will be passed through the part of the body which needs to be examined, this is often skeletal sites, such as your lower spine and hip joint, to check for weak bones, but more than one part of your body may be scanned, as bone density can vary in different bones.
Bone density tests are available through an NHS referral. The scan usually takes 10 to 20 minutes, and you can go home once it’s done.

What is Osteoporosis?
Osteoporosis is a lack of bone density which weakens the bones, making them more likely to break. A diagnosis of osteoporosis is not usually made until a fall or sudden impact causes a broken bone or osteoporotic fracture and then Bone density testing is done. The most common injuries which show signs of osteoporosis are hip fracture, a break in the vertebrae(spinal bones) or broken wrists; however, breaks from osteoporosis can happen in other bones. Osteoporosis doesn’t cause unusual pain until a bone is fractured or broken. Other signs of osteoporosis can be a bent forward posture; this happens when the bones in the spine have been broken and have more trouble supporting the body’s weight.
The age of patients diagnosed with osteoporosis is generally between 50 -90. Adult women in the age bracket are more likely to be diagnosed with osteoporosis as they have lighter, thinner bones and an average longer lifespan.
How does osteoporosis affect day-to-day life?
Having osteoporosis does not mean you’ll definitely experience a fracture or bone break. However, it does mean you’ll likely need to take measures to reduce your risk of falls or knocks.
- Check your home for hazards such as loose carpets and rugs, clutter on the floor, uneven steps, loose wires and cords, or large pieces of furniture that sticks out into walkways
- Make sure you have a balanced diet that’s rich in all major food groups. The NHS has a good guide on bone healthy diets.
- Fear of falls or injury can have a big impact on some people and limit how they spend their time. Speaking to your GP or an independent counsellor can help with worries.
- Keep up with eye and hearing tests to help you stay as sharp as possible when moving around and avoiding hazards
- Ask your GP about an occupational therapist visit. They can help identify mobility aids and support such as grab rails and bathroom safety.
How does osteoporosis affect someone’s social life?
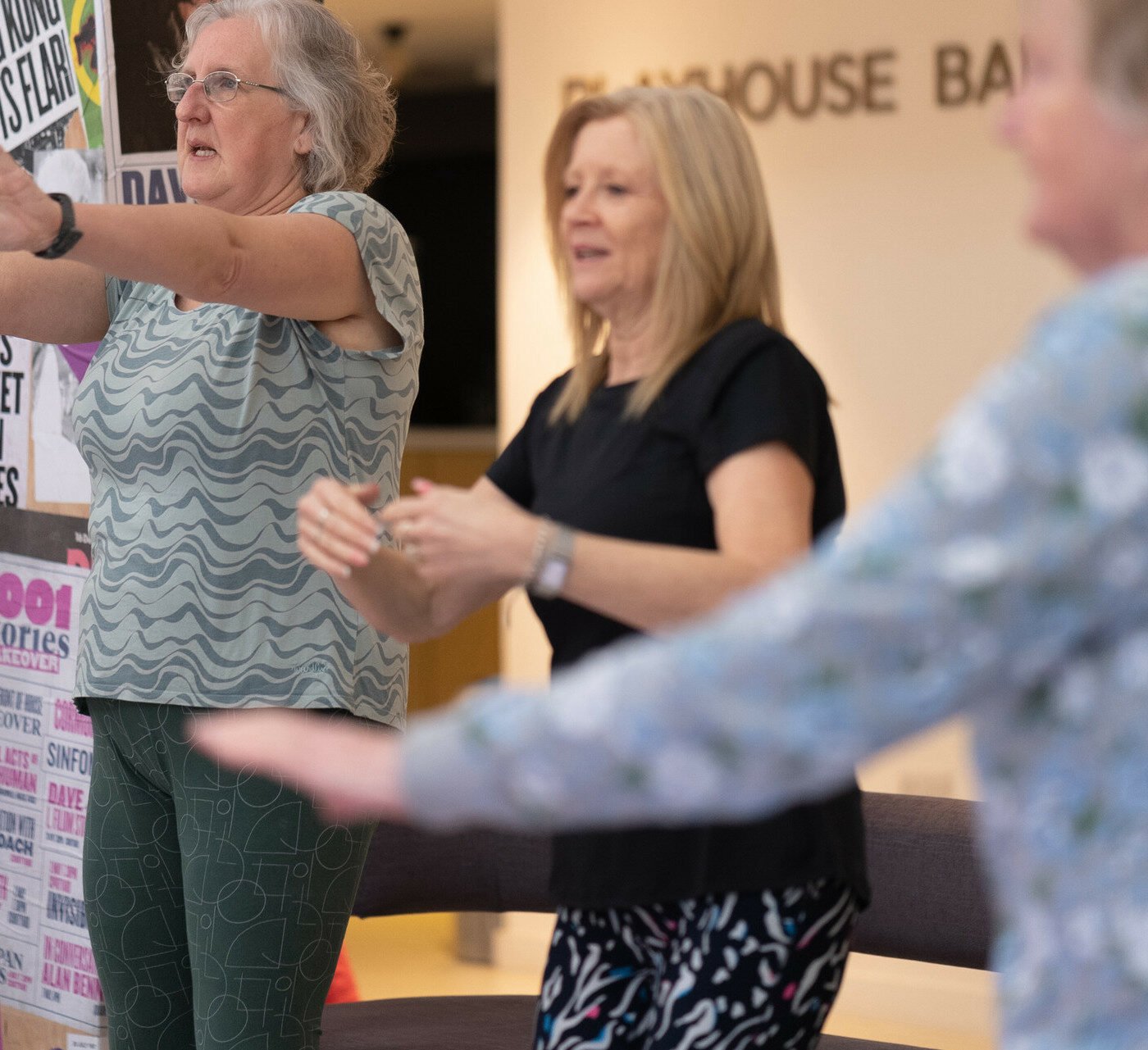
There’s no reason why osteoporosis should limit your social life, it may just mean making small changes that accommodate your mobility levels. Many gyms and community centres offer gentle exercise and activity classes, so always ask if you’re keen to join one if it’s the right level for you.
If you’re no longer able to enjoy a particular sport or hobby, use this as an opportunity to try something new. Spending time in the garden, joining a book club, playing bingo or board games, or getting out for a coffee and a chat are great ways to see friends and stay social, without putting unnecessary pressure on your bones.
For some inspiring stories from people who are living an active social life with osteoporosis, take a look at Health Talks interviews.
Living long and well – the role of physiotherapy in later life
As CEO of The Chartered Society of Physiotherapy, Karen Middleton is passionate about the role physiotherapy has to play in enabling people to live long and live well. We talked to her about how crucial it is to stay active for optimum health and life experienceHow can I improve my T-score and prevent osteoporosis?
Some people have unchangeable risk factors for osteoporosis. However, lifestyle choices can influence your bones’ health and reduce bone loss. For older people who require regular professional support, a carer can help ensure the following positive habits are part of the daily routine.
Exercise
The World Health Organisation recommends that the average adult between the ages of 18-64 should do at least 1.25 – 5 hours of physical activity a week, and to reduce the detrimental effects of high levels of a sedentary lifestyle. All adults should aim to do more than the recommended levels of moderate to vigorous physical activity. They suggest the same for adults aged 65 years and over; however, they should also do varied activities focusing on functional balance and strength training on three or more days to enhance functional capacity and prevent likelihood of falls.
Healthy Eating
A healthy diet is vital for every aspect of our lives, including maintaining healthy bones and preventing osteoporosis.
To maintain healthy bones, an emphasis is put on consuming enough calcium. 700mg of calcium daily is recommended, which is easily achieved through a healthy diet. Calcium-rich foods include leafy greens, salmon, different types of beans, dairy products and juices such as Orange juice.
Vitamin D
The body absorbs vitamin D from the sun, food, and supplements. Vitamin D is vital for healthy bones as it helps your body absorb calcium.
Being in the sun can trigger Vitamin D production, however, you can also consume the daily recommended ten micrograms of Vitamin D a day from food such as; oily fish (Salmon, sardines etc.), egg yolks, some breakfast cereals and red meat. If you find it challenging to get your vitamin D needs from these foods alone, you can take daily supplements of Vitamin D; however, it’s always best to seek medical advice if you’re thinking about adding supplements to your diet.
Drinking less alcohol and stopping smoking
The NHS recommendation is not to drink more than fourteen units of alcohol a week; this is important for many reasons, however, when it comes to bone health, excessive alcohol consumption can decrease the body’s absorption of calcium and vitamin D, which are vital for bone health. Smoking has also been linked to increased chances of poor bone health as it affects body weight, vitamin D levels, and many other negative health effects.
This article is for informational purposes only and not to be taken as medical advice. For medical advice, always consult your GP.
Read more care guides

How to prepare for a live-in caregiver
Care at home: how to prepare the home for a live-in caregiver A live-in carer can make a massive difference to your loved one’s quality

6 tips for finding the right live-in carer
Finding the right live-in carer is a significant and deeply personal decision, impacting your loved one and the entire family. You’re seeking someone trustworthy, compassionate,

The cost of care – everything you need to know
The true cost of care – everything you need to know Discover the true cost of care and explore your funding options with our care

Understanding autism in older adults
While Autism is usually diagnosed in childhood, an increasing number of older adults are being formally diagnosed in later life. Masking autism symptoms can result

A guide to speaking with a loved one about home care
Why do older adults resist care? A guide to speaking with a loved one about home care Bringing up the topic of care at home

How to choose the right personal alarm for seniors: A comprehensive guide
Personal alarms for elderly Discover how personal alarms work, who they’re best suited to, and how they provide greater peace of mind to older people